ABSTRACT
Patients with short bowel syndrome (SBS) have a high risk of developing parenteral nutrition (PN)-associated complications. Therefore, diet or enteral nutrition and PN should be modified to limit such complications. N balance analysis is a method of calculating the amount of protein required to achieve N equilibrium in the body based on intake and excretion. It is important to reduce dependence on PN and achieve the recommended range of N balance 2–4 g with an appropriate diet. We report a recent experience with nutrition modification using N balance analysis and suggest it as a useful method to reduce dependence on PN in nutrition management of SBS patients and in continuing active intestinal rehabilitation.
-
Keywords: Short bowel syndrome; End-jejunostomy; Nitrogen balance; Nutrition care
INTRODUCTION
Short bowel syndrome (SBS) refers to a condition in which the small bowel (SB) remains less than 200 cm from the ligament of Treitz [
1]. This shorter than normal SB has less surface area for absorption of nutrients, resulting in difficulty maintaining fluid and electrolyte homeostasis [
1,
2]. Among the anatomical phenotypes of SBS, end-jejunostomy requires permanent parenteral nutrition (PN) and is the most difficult to manage [
2,
3]. Long-term PN supply can cause problems such as intestinal failure-associated liver disease (IFALD), catheter-related blood stream infection (CRBSI), and reduced quality of life [
3,
4]. To prevent these complications, PN dependence should be reduced by improving intestinal adaptation through diet or enteral nutrition (EN). Eunpyeong St. Mary’s Hospital has introduced a nutrition care process that reduces PN dependence using nitrogen (N) balance analysis in SBS patients with end-jejunostomy.
CASE
Patient profile
A 64-year-old man (body weight: 59 kg; body mass index: 21.8 kg/m2) was admitted to Eunpyeong St. Mary’s Hospital for SB transplantation on February 22, 2021. He suffered SB and colon ischemia due to superior mesenteric artery (SMA) occlusion, for which he underwent resection of the SB with right colon on January 17, 2021 (remaining bowel: jejunum 30cm, ascending colon, end-jejunostomy status).
Nutrition management
On postoperative day (POD) #18 at the original hospital, the patient started sipping thin rice gruel and other liquids but maintained fasting as jejunostomy output (JO) increased to 6 L/day. Laboratory data showed dehydration, so intravenous (IV) fluid and oral rehydration solutions (ORS, Pedira powder: 6.264 g, containing 5 g of glucose, 0.432 g of potassium citrate, 0.41 g of sodium chloride, and 0.172 g sodium citrate) were supplied.
An individually adjusted oral diet was started for intestinal adaptation (hospital day [HD] #15). Hydration was performed with ORS 500 mL and free water 500 mL, but JO continued greater than 3 L/day (
Table 1), so 1 L of hydration was performed only with ORS instead of water. As JO decreased, porridge was added to his diet (HD #18), and about 40% of total calories were supplied as fat according to the American Society for Parenteral and Enteral Nutrition (ASPEN) guidelines.
Table 1Progression of physical and biochemical findings of the patient
Table 1
|
Parameters |
Normal |
Admission (Feb. 22, 2021) |
HD #15 |
HD #29 |
HD #36 |
HD #39 |
HD #43 |
HD #46 |
HD #50 |
HD #53 |
HD #71 |
|
Body weight (kg) |
53.3–65.1 |
57.4 |
59.4 |
59.95 |
60.95 |
61 |
61.85 |
62.05 |
62.85 |
61.2 |
59.6 |
|
I/O |
|
|
|
|
|
|
|
|
|
|
|
|
Intake (mL) |
- |
677 |
6,050 |
4,980 |
4,378 |
5,417 |
4,120 |
4,794 |
2,364 |
4,602 |
4,358 |
|
Total output (mL) |
- |
0 |
5,855 |
4,200 |
4,300 |
3,800 |
3,250 |
4,200 |
2,650 |
3,100 |
3,500 |
|
JO (mL) |
- |
0 |
3,955 |
2,500 |
2,400 |
2,800 |
2,050 |
3,450 |
1,700 |
1,850 |
2,400 |
|
Laboratory data |
|
|
|
|
|
|
|
|
|
|
|
|
Urea nitrogen (mg/dL) |
8.0–20.0 |
24.9 |
14.2 |
12.8 |
12.8 |
15 |
13.8 |
13.8 |
5.9 |
9.2 |
21.2 |
|
Creatinine (mg/dL) |
0.61–1.20 |
0.77 |
0.51 |
0.55 |
0.57 |
0.54 |
0.58 |
0.65 |
0.57 |
0.58 |
0.72 |
|
Calcium (mg/dL) |
8.8–10.6 |
8.9 |
8.4 |
8.3 |
8.2 |
8.4 |
8.4 |
8.6 |
8.4 |
8.6 |
9.1 |
|
Phosphorus (mg/dL) |
2.5–4.5 |
3.9 |
3.7 |
2.7 |
3.2 |
- |
3.7 |
- |
3.5 |
3.8 |
4 |
|
Sodium (mmol/L) |
136–146 |
134 |
136 |
139 |
138 |
139 |
139 |
139 |
141 |
141 |
141 |
|
Potassium (mmol/L) |
3.5–5.1 |
4.3 |
3.9 |
4.2 |
4.2 |
3.6 |
4.3 |
4.3 |
3.1 |
3.2 |
4.2 |
|
Chloride (mmol/L) |
101–109 |
99 |
106 |
105.2 |
106.8 |
107.8 |
107.4 |
108.3 |
108.1 |
108 |
108.3 |
|
Total bilirubin (mg/dL) |
0.3–1.2 |
2.07 |
1.54 |
1.53 |
1.5 |
1.94 |
2.11 |
2.76 |
2.9 |
2.98 |
3.08 |
|
Direct bilirubin (mg/dL) |
0–0.2 |
0.74 |
0.48 |
0.47 |
0.39 |
- |
0.56 |
0.67 |
0.78 |
- |
- |
|
AST (U/L) |
0–50 |
43 |
37 |
43 |
43 |
41 |
43 |
51 |
39 |
32 |
48 |
|
ALT (U/L) |
1–50 |
56 |
48 |
61 |
70 |
74 |
68 |
69 |
67 |
48 |
75 |
|
Alkaline phosphatase (U/L) |
30–120 |
278 |
174 |
189 |
173 |
163 |
178 |
198 |
142 |
137 |
167 |
|
WBC count (109/L) |
4.0–10.0 |
9 |
5.1 |
4.5 |
4.2 |
4.6 |
3.5 |
4.8 |
3.9 |
3.9 |
4.3 |
|
Hemoglobin (g/dL) |
12.5–18.0 |
12.3 |
9.8 |
9.9 |
9.6 |
9.7 |
9.3 |
10.4 |
9.5 |
9.6 |
11.2 |
|
Hematocrit (%) |
38.0–54.0 |
37 |
29.3 |
29.7 |
28.8 |
28.8 |
27.8 |
31.2 |
28.7 |
29.4 |
33.6 |
|
Platelet count (109/L) |
150–450 |
213 |
243 |
189 |
178 |
172 |
162 |
170 |
148 |
157 |
135 |
|
Lymphocytes (%) |
20–44 |
46.1 |
53.5 |
52 |
57 |
58.9 |
56 |
61 |
55.1 |
58 |
55.6 |
|
ANC (109/L) |
0.0–0.5 |
4 |
1.6 |
1.53 |
1.39 |
1.2 |
0.91 |
0.96 |
1.3 |
1.33 |
1.4 |
Based on his condition, his oral diet was composed of high fat, low fiber, and low water contents (HD #18). As ORS compliance was low, hydration was supplied with ORS 500 mL and free water 500 mL (HD #24). Gradually, the amount of oral diet was increased by 50 g to reach 700 g/day (HD #46).
However, JO which had maintained an average of 2,700 mL/day increased to an average of 3,800 mL/day, and the levels of liver function parameters (bilirubin, aspartate transaminase [AST], alanine transaminase [ALT]) were constantly higher than normal, confirming overall steatosis and fibrosis, as shown on liver ultrasound (
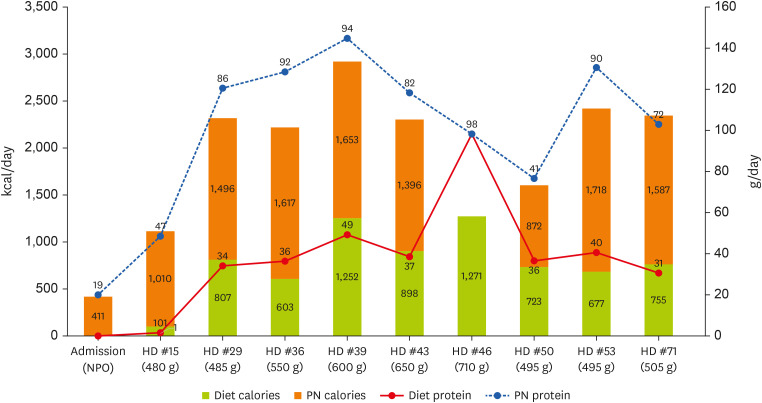
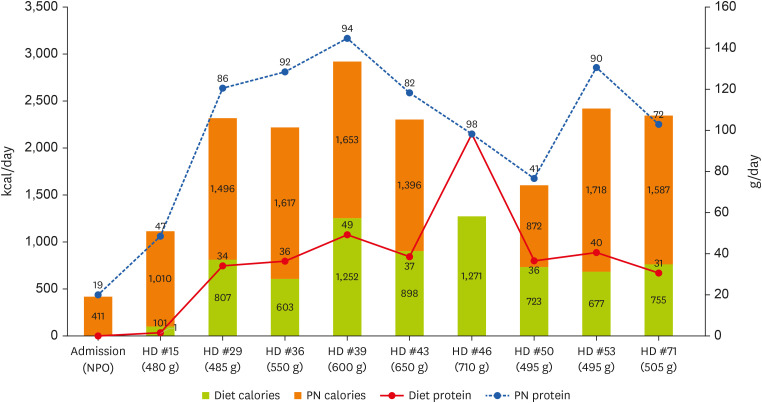
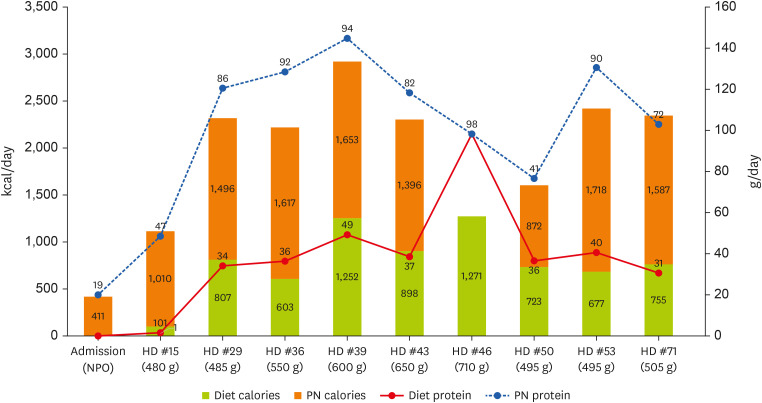
Table 1). Accordingly, the oral diet was reduced to 500 g/day, and the fat ratio was decreased to 30% of the total calories (HD #50). In addition, to reduce the amount of fat supplied via IV, daily commercial 3-in-1 PN (1,078 kcal, 125 g of carbohydrate, 50 g of protein, 38 g of fat with addition of electrolytes) was provided twice per week, and commercial 2-in-1 PN (1,169 kcal, 250 g of carbohydrate, 50 g of protein with addition of electrolytes) was supplied five times per week (HD #53). The process of his overall nutrition care is summarized in
Table 2, and the energy and protein intakes from his diet and PN are shown in
Figure 1.
Table 2Summary of the nutrition care in short bowel syndrome patient
Table 2
|
Hospital course |
Diet intake |
Diet intake + PN (% of requirement) |
Nutrition management |
|
Admission (Feb. 22, 2021) |
NPO |
Calories: 411 kcal/day (20%) |
[Initial nutritional assessment]
|
|
Protein: 19 g/day (21%) |
Severe malnutrition (based on ASPEN/AND malnutrition criteria) |
|
[Nutrition requirement]
|
|
Energy goal: 2,100 kcal/day (IBW × 35 kcal/kg) |
|
Protein requirement: 90 g/day (IBW × 1.5 g/kg) |
|
• 6 L/day of JO continues before admission |
|
• Dehydration status at the time of admission (Na-K-Cl 134-4.3-99.0, BUN/Cr 24.9/0.77) |
|
→ Commercial ORS recommend starting with 1 L/day and increasing to 2–3 L/day |
|
HD #15 |
Calories: 101 kcal/day |
Calories: 1,011 kcal/day (53%) |
[Diet order]
|
|
Protein: 1.4 g/day |
Protein: 47 g/day (52%) |
: LD 500 g/day (HD #15) |
|
C:P:F = 94:06:00 |
• Rice water (6 times/day) |
|
• ORS 500 mL + Free water 500 mL |
|
→ ORS 1 L/day, due to JO continues more than 3 L (HD #17) |
|
HD #29 |
Calories: 807 kcal/day |
Calories: 1,614 kcal/day (115%) |
[Diet order]
|
|
Protein: 34 g/day |
Protein: 75 g/day (121%) |
: SD 500 g/day |
|
C:P:F = 35:17:48 |
• Porridge (6 times/day) (HD #18) |
|
(High fat, low fiber, low water content diet) |
|
• Add protein powder |
|
• Fat sources: butter, mayonnaise (poor compliance to sesame oil and perilla oil) |
|
• Changed back to ORS 500 mL + Free water 500 mL (HD #24) (poor compliance of ORS) |
|
HD #36 |
Calories: 603 kcal/day |
Calories: 1,617 kcal/day (106%) |
[Diet order]
|
|
Protein: 36 g/day |
Protein: 91.9 g/day (142%) |
: SD 550 g/day |
|
C:P:F = 42:19:39 |
• There is no change in JO volume and good dietary compliance, SD recommend to increase 600 g/day. |
|
HD #39 |
Calories: 1,252 kcal/day |
Calories: 1,653 kcal/day (138%) |
[Diet order]
|
|
Protein: 49 g/day |
Protein: 93.6 g/day (158%) |
: SD 600 g/day |
|
C:P:F = 43:16:41 |
• There is no change in JO volume and good dietary compliance, SD recommend to increase 650 g/day. |
|
HD #43 |
Calories: 898 kcal/day |
Calories: 1,396 kcal/day (109%) |
[Diet order]
|
|
Protein: 37 g/day |
Protein: 81.6 g/day (132%) |
: SD 650 g/day |
|
C:P:F = 47:17:37 |
• There is no change in JO volume and good dietary compliance, SD recommend to increase 700 g/day. |
|
HD #46 |
Calories: 1,271 kcal/day (60%) |
- |
[Diet order]
|
|
Protein: 102 g/day (113%) |
: SD 700 g/day |
|
C:P:F = 26:32:42 |
• After increasing to SD 700 g/day, JO increases |
|
HD #50 |
Calories: 723 kcal/day |
Calories: 872 kcal/day (76%) |
[Diet order]
|
|
Protein: 40 g/day |
Protein: 40.8 g/day (90%) |
: SD 500 g/day |
|
C:P:F = 46:22:32 |
• 4/11 pitting edema observed |
|
• SD 500 g/day reduction and fat ratio adjustment (40% → 30%) with JO increase and r/o steatosis |
|
HD #53 |
Calories: 677 kcal/day |
Calories: 1,718 kcal/day (114%) |
[Diet order]
|
|
Protein: 40 g/day |
Protein: 90 g/day (144%) |
: SD 500 g/day |
|
C:P:F = 48:24:28 |
• Changing the PN formulation to reduce fat supplied to IV |
|
→ 3-in-1 PN supplied daily was reduced to twice a week, and 2-in-1 PN was supplied 5 times a week (HD #53) |
|
HD #71 |
Calories: 755 kcal/day |
Calories: 1,667 kcal/day (115%) |
[Nutritional assessment]
|
|
Protein: 31 g/day |
Protein: 70 g/day (112%) |
Severe malnutrition (based on ASPEN/AND malnutrition criteria) |
|
C:P:F = 48:17:35 |
[Diet order]
|
|
: SD 500 g/day |
Figure 1
The energy (kcal/day) and protein (g/day) intakes from diet and PN.
PN, parenteral nutrition; HD, hospital day.
N balance analysis
An N balance analysis was used to evaluate the patient's protein absorption. The first urine on the designated date was discarded, and the urine was collected in a specimen container for 24 hours until the first urine the next day, the total amount of the specimen was recorded, and only a small amount (30–50 mL) was collected and sent to the laboratory. Urea N measured by an enzymatic rate method (Beckman Coulter AU5800 System; Beckman Coulter, Brea, CA, USA). In the reaction, urea was hydrolyzed by urease to ammonia and carbon dioxide. Glutamate dehydrogenase catalyzes the condensation of ammonia and α-ketoglutarate to glutamate with the concomitant oxidation of reduced β-nicotinamide adenine dinucleotide to β-nicotinamide adenine dinucleotide.
The N output is known to increase under stoma or fistula condition. To address this, we measured the N level directly from the total 24-hour JO. Two well mixed specimen containers (10 mL, each) from 24-hour JO were sent to the laboratory, and the container had informed as the registration number and the name of patient, the total amount of specimen. The phased of oral diet supplied only, however, N could not be determined from JO; instead, we used the N of JO results observed under other conditions.
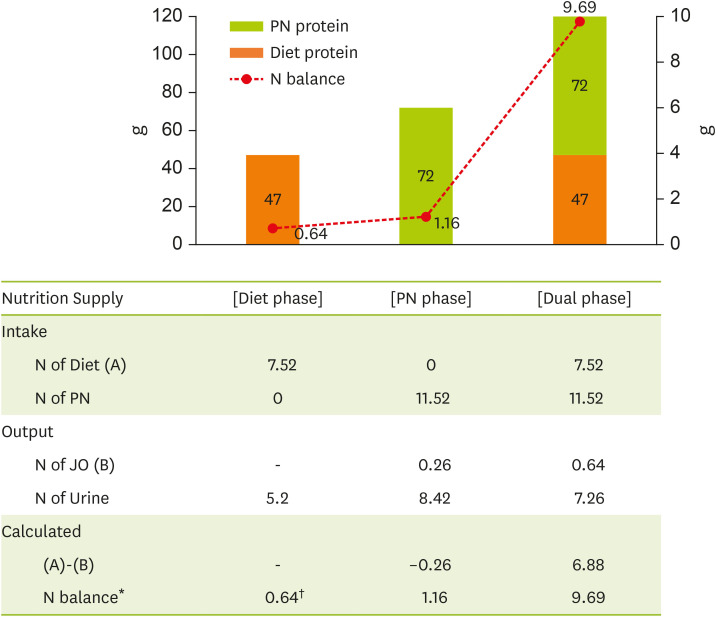
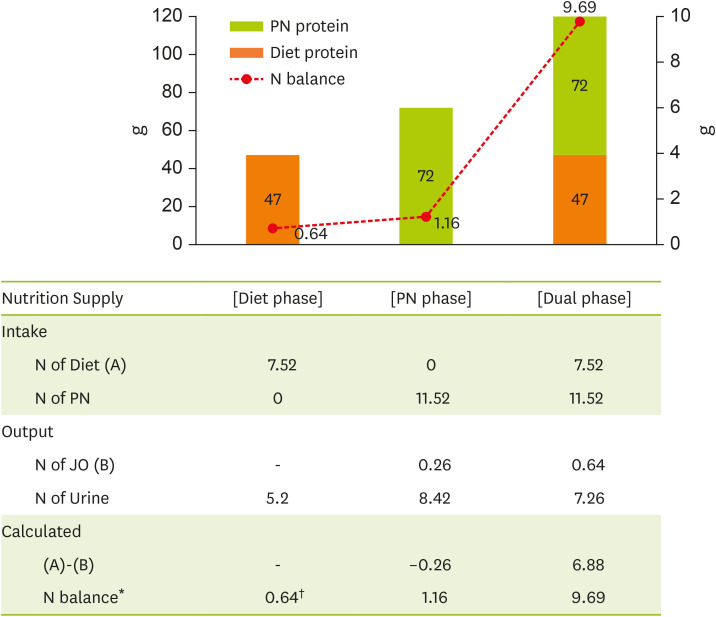
The N balance was calculated as the difference between N intake (N in diet and PN) and N output (N in JO and urine) [
2]. The measurement was performed 3 times under different conditions depending on presence of oral diet or PN (Diet, PN, and Dual phases) (
Figure 2).
Figure 2
Nitrogen balance under diet and parenteral nutrition (PN).
PN, parenteral nutrition; N, nitrogen; JO, jejunostomy output.
*N balance = N intake-N Output [{Urine Urea N (mg/100 mL) × 24 Hours Urine Volume (L/day)} + 20% of Urinary Urea Loss + N of JO].
†Calculated from JO data of Dual phase.
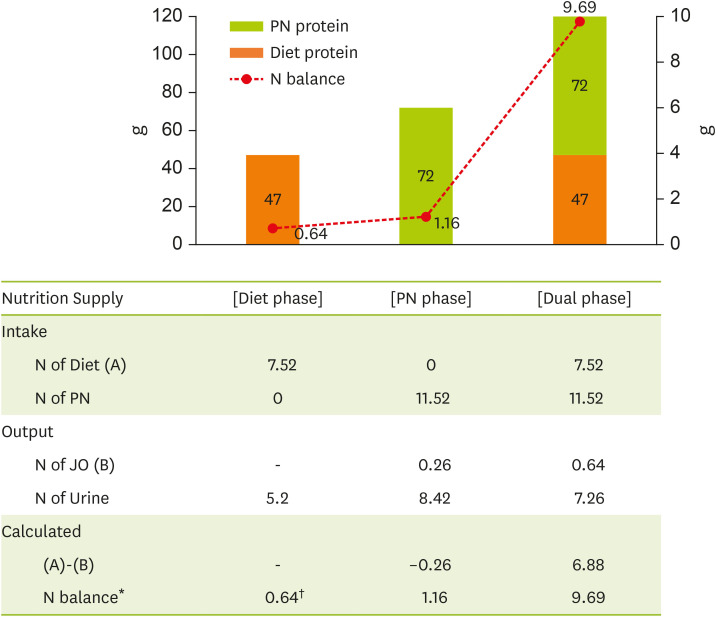
The measurement showed a positive N balance under all conditions, 0.64 g when under oral diet only, 1.16 g when only PN was supplied, and 9.69 g when both oral diet and PN were combined.
DISCUSSION
SBS is not common in clinical practice, so little is known about related nutrition management. In particular, end-jejunostomy is difficult to manage, and proper nutrition is necessary for a good prognosis.
The presented patient has end-jejunostomy with a remaining SB of 30 cm and requires permanent PN. However, long-term PN can lead to serious complications such as catheter infection, sepsis, venous thrombosis, and liver failure [
5].
Remnant SB undergoes adaptation involving morphological and functional changes over two years after resection [
6,
7]. Oral diet or EN is started for adaptation of the remaining SB to stimulate mucosal hyperplasia by direct contact with intestinal epithelial cells, promote gastrointestinal mucosal activity, and increase pancreatic-biliary secretions [
1,
8].
The present patient had been supplied with PN in a long-term fasting state prior to admission and showed elevated levels of liver function parameters (bilirubin, AST and ALT). We started individualized diet modification for intestinal adaptation as a first-line therapy. Various nutrients are absorbed by different areas of the SB [
9], with fat and protein absorption shown to be easy in SBS patients with end-jejunostomy [
2,
7]. Therefore, his diet consisted primarily of high fat, low fiber, and low water contents. During the diet as porridge 6 times a day was low compliance for patient because of monotonous pattern, so the dietitian planed diet composed of rice, bread, potatoes, eggs, tofu, and plain yogurt, and butter and mayonnaise were used as fat sources. The nutrition data and the ratio of macronutrients are shown in
Table 2.
The levels of his liver function parameter continued to increase, and steatosis and fibrosis were observed on liver ultrasound. Steatosis is a condition in which at least 5% of the liver’s weight is comprised of fat and is caused by a high-calorie, high-fat diet [
10]. Steatosis can occur in patients with chronic intestinal failure maintaining long-term PN, which leads to IFALD [
11]. In order to improve liver function and steatosis, the amount of diet and fat ratio was reduced, and also reduced fat supplied via intravenous injection by changing the PN formulation. Although not shown in
Table 1, the levels of liver function parameters decreased after these interventions (HD #78, total bilirubin 2.77 mg/dL, ALT 63 U/L).
The N balance results were measured three times to evaluate protein absorption (
Figure 2) and were highest (9.69 g) with oral diet and PN combined compared to oral diet or PN fed alone. When comparing the PN and Dual phases that supplied the same PN, the N balance difference was large, which is thought to be due to the presence or absence of diet. Subtracting the N excreted as JO from the N consumed from the diet predicts the N remaining in the body. Although it is very careful to predict dietary nutrient absorption, it is estimated that 6.88 g of N (43 g of protein) is absorbed from the remaining SB when intuitively interpreting the results (A)-(B) Dual phase.
The N balance analysis is the most direct method for estimating protein requirement, which is recommended at +2–4 g for anabolism [
12]. During the Dual phase, protein was oversupplied in excess of the recommended range of N balance (9.69 g). Based on these results, the PN supply was adjusted while maintaining the oral diet to decrease PN dependence without significant weight loss.
Though it has been shown that N excretion is higher in patients with stoma/fistula, lack of data complicates evaluation of nutritional status and protein requirement. There are scarce data related to N balance in SBS patients, so nutrition care of such patients is of great importance. This case suggests the need for intestinal rehabilitation through supply of nutrients through the gastrointestinal tract to SBS patients. However, as this condition is rare, it is not easy to obtain consistent data, and the results will vary based on individual differences. Nevertheless, N balance analysis can be included in the various approaches needed for nutritional care of SBS patients. SB absorption can be approximated through N balance analysis, allowing provision of more appropriate nutritional care. This process is thought to ultimately contribute to reducing PN dependence and the risk of side effects from PN supply in SBS patients.
NOTES
-
Conflict of Interest: The authors declare that they have no competing interests.
-
Author Contributions:
Conceptualization: Sim S, Kim J, Park J, Cheon J.
Data curation: Kim A, Sim S.
Formal analysis: Kim A, Sim S, Kim J.
Investigation: Sim S, Lee J.
Methodology: Park J.
Project administration: Kim A.
Supervision: Kim A, Kim J.
Validation: Hwang J.
Visualization: Kim A.
Writing - original draft: Kim A, Kim J.
Writing - review & editing: Kim A, Kim J, Hwang J.
REFERENCES
- 1. Corrigan ML, Roberts K, Steiger E. Adult short bowel syndrome. Cambridge: Academic Press; 2019.
- 2. Limketkai BN, Hurt RT, Palmer LB. The ASPEN adult nutrition support core curriculum. 3rd ed. Silver Spring (MD): American Society for Parenteral and Enteral Nutrition (ASPEN); 2017.
- 3. Parrish CR, DiBaise JK. Managing the adult patient with short bowel syndrome. Gastroenterol Hepatol (N Y) 2017;13:600-608.
- 4. Bielawska B, Allard JP. Parenteral nutrition and intestinal failure. Nutrients 2017;9:466.
- 5. Gong JF, Zhu WM, Yu WK, Li N, Li JS. Role of enteral nutrition in adult short bowel syndrome undergoing intestinal rehabilitation: the long-term outcome. Asia Pac J Clin Nutr 2009;18:155-163.
- 6. Wall EA. An overview of short bowel syndrome management: adherence, adaptation, and practical recommendations. J Acad Nutr Diet 2013;113:1200-1208.
- 7. Matarese LE, O’Keefe SJ, Kandil HM, Bond G, Costa G, Abu-Elmagd K. Short bowel syndrome: clinical guidelines for nutrition management. Nutr Clin Pract 2005;20:493-502.
- 8. Thompson JS, Rochling FA, Weseman RA, Mercer DF. Current management of short bowel syndrome. Curr Probl Surg 2012;49:52-115.
- 9. Gropper SS, Smith JL, Groff JL. Advanced nutrition and human metabolism. Boston (MA): Cengage Learning; 2008.
- 10. Nassir F, Rector RS, Hammoud GM, Ibdah JA. Pathogenesis and prevention of hepatic steatosis. Gastroenterol Hepatol (N Y) 2015;11:167-175.
- 11. Jordan T, Popovič P, Rotovnik Kozjek N. Liver steatosis in adult patients on home parenteral nutrition. Eur J Clin Nutr 2020;74:255-260.
- 12. Korean Dietetics Association (KDA). Manual of medical nutrition therapy. 3rd ed. Seoul: KDA; 2013.
 , Sunglee Sim1
, Sunglee Sim1 , Jeeyeon Kim1
, Jeeyeon Kim1 , Jeongkye Hwang2
, Jeongkye Hwang2 , Junghyun Park2
, Junghyun Park2 , Jehoon Lee3
, Jehoon Lee3 , Jeongeun Cheon4
, Jeongeun Cheon4